All Austrian Health Insurance Funds & Private
Group-Practice Internist-Nord.at
Syeda | Gregor | Kowatschitsch | Al Bahloul
Sopira | Pakzad | Promintzer-Schifferl
Specialists for Internal Medicine, Cardiology, Gastroenterology, Diabetology and Hepatology


Cardiovascular Diseases
Cardiovascular disease is a general term that describes all the conditions of the heart or blood vessels.
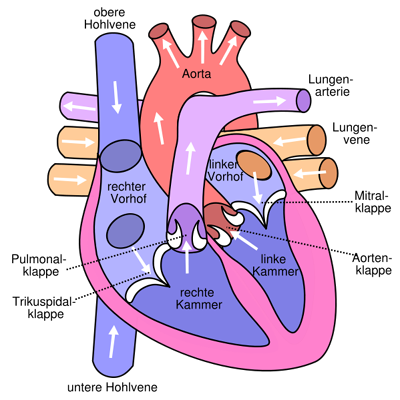
How does my heart work?
The heart is the engine of our life. It is located in the centre of the chest and it is about the size of a fist and has a mass of between 260 grams in females and 350 grams in males. It is divided into two halves by the septum. Each half consists of two chambers, a superior atrium and an inferior ventricle. The atria are the receiving chambers for the blood flowing back into the heart. From the atria the blood flows into the ventricles, which are the pumping stations of our cardiovascular system and whose function it is to supply the vessels (arteries, veins, and capillaries) with blood. Arteries are vessels that carry blood away from the heart, whereas veins carry blood towards the heart. Exchange of oxygen and nutrients to the organs and tissue takes place in the fine capillaries connecting arteries and veins.
Frequent cardiological conditions
- Coronary heart disease
- Cardiac insufficiency
- Valvular defect
- Cardiac arrhythmia
- High blood pressure (arterial hypertonia)
- Peripheral arterial occlusive disease
- Stroke
- Varicose veins
- Thrombosis
Coronary heart disease
Coronary heart disease is a condition of the coronary heart vessels (coronary arteries). Its most common cause is arteriosclerosis, where the artery wall thickens due to plaque, causing hardening, as well as a decrease in the vessel’s cross section. The result is insufficient blood supply and thus insufficient oxygen supply for the heart muscle. This leads to disaccord between oxygen need and supply, which is called ischemia or coronary insufficiency.
The cardinal symptom of coronary heart disease is angina pectoris (chest tightness). As the disease progresses, the chances for attendant symptoms such as cardiac arrhythmia or cardiac insufficiency, as well as life threatening complications like heart attack or sudden cardiac death increase.
Coronary heart disease is a chronic condition, progressing slowly over years and decades. There is no cure for this condition; however, it is possible to fight aggravation by avoiding or pharmaceutically treating risk factors. Additionally, there are certain therapeutic interventions by means of catheter or surgery to treat coronary heart disease. With its acute manifestations, coronary heart disease is one of the main causes of death in developed nations.
Stable angina pectoris
In this case stable denotes that the angina pectoris always occurs under the same circumstances. There are four different stages, with each of which the pain and the constraints entailed with it, increase.
- Stage 1 – slight form, no medical conditions in daily life
- Stage 2 – daily activities are only slightly limited. Conditions only during hasty ascending of stairs, walking uphill, cold and headwind.
- Stage 3 – daily activities very limited, e.g. walking up one staircase
- Stage 4 – heavy form with conditions during rest.
Unstable angina
In this case unstable refers to the fact that conditions might change or worsen. A distinction is made by:
- Rest angina – pain attacks usually last more than 20 minutes
- Progressive angina – angina pectoris where symptoms worsen within a period of 2 months by one grade.
Symptoms – typical angina pectoris
- Type of pain: pressure in the chest region, tightness in the chest, burning session or choking
- Location of pain: above the breastbone, upper central abdomen and throat, jaw, left should and arm, left blade bone
Symptoms – atypical angina pectoris
There might also be atypical conditions, which might occur during certain positions. Pain might only occur at night or can vanish during physical exercise.
Heart attack
Heart attacks are today’s most common cardiovascular problems. The first signs of a heart attack are usually:
- Persistent pain in the chest
- Shortage of breath, nausea and vomiting
- Paleness, cold sweat
- Sudden circulatory collapse with or without loss of consciousness
The earlier a patient receives treatment, the higher the chances of survival. The first measure is the attempt to remove the obstruction or occlusion of the coronary blood vessel. Immediate treatment can prevent sustained damage.
Treatment options
Medical treatment of the risk factors
Dilatation (PTCA) and stent implantation
PTCA means percutaneous transluminal coronary angioplasty and refers to the possibility of widening a narrowed or obstructed coronary blood vessel by means of intracardiac catheter (coronary angioplasty). In coronary angioplasty access is gained through the ingenual artery and a contrasting medium is injected to depict the coronary arteries. Should an obstruction or stenosed area become visible, PTCA is the next step. Usually a stent (stainless steel support tube for the artery) is implanted during this procedure, to keep the vessel open. A stent is a small tube made out of wire mesh and permanently remains in the blood vessel.
Aortocoronary bypass (ACBP)
Aortocoronary bypass (ACBP), also coronary artery bypass graft (CABG) surgery is the most frequently performed heart surgery in developed countries. It is the means of treatment for patients with more than one stenosed area and is applied to ensure long-term survival and improve quality of life. The procedure is indicated when stenosed areas have been located through coronary angiography and when these areas cannot be treated with other interconventional measures. During the procedure arteries from healthy areas of the body (e.g. thoracic artery, crural vein, and antebrachial vein) are used to bridge obstructed or stenosed areas. The chest is opened, the patient connected to a heart-lung machine and the bridge is sewn on to the coronary arteries beyond the blockages and the other end is attached to the aorta using thin thread.
Cardiac insufficiency
Cardiac insuffficiency is a pathological state where the heart can no longer pump sufficient blood through the body. Thus, the heart can no longer sustain blood flow to the organs.
The onset of this condition may be sudden with hours or days. This is referred to as acute cardiac insufficiency and presents a medical emergency.
Chronic cardiac insufficiency, on the other hand, develops slowly over months and years. It may become an acute condition if additional factors such as infection, anemia, a blood pressure crisis or an arrhythmia have a negative impact onto the already weakened heart. We speak of left cardiac insufficiency if the left ventricle is affected and of right cardiac insufficiency should the right ventricle be mainly affected. In case both ventricles are affected, the condition is referred to as global cardiac insufficiency.
Causes of cardiac insufficiency are for example
- previous heart attack
- long history of high blood pressure
- inflammation of the heart muscle
- diseases related to the heart valve
- extensive consumption of alcohol
- storage diseases
Symptoms
Symptoms of chronic cardiac insufficiency develop gradually over time. Patients will notice that they feel weaker. Initially this will only be noticeable during heavy exercise, later on also during light exertion. They will feel tired and exhausted quickly and get out of breath easily. Water retention, primarily in the feet, ankles and lower legs is another possible symptom.
Treatment
A weak heart is not just a sign of age. Early and consistent treatment is key in avoiding serious consequences or at least delays and reduces symptoms.
Treatment largely depends on the underlying cause. If possible the direct cause will be eliminated. It will be necessary and important to change your lifestyle. Additionally, there is medication available to relieve and strengthen the heart. Depending on the present situation, treatment options include placing a pacemaker or a stent to improve blood flow in the heart, bypass surgery, valve surgery and in severe cases heart transplantation.
Valvular defects
Heart valves are structures of connective tissue between the atria and the ventricles of the heart (atrioventricular valves: tricuspid valve, mitral valve) and separate ventricle and larger vessels (semilunar valves: aortic valve and pulmonary valve). A distinction is made between congenital and acquired valvular defects.
Congenital defects are malformations at the time of birth; the condition of the valve in question usually worsens over the course of life. Acquired defects are caused by inflammations of the valves (endocarditis) or by increasing calcification.
Treatment options are either medication or two types of surgery:
Reconstruction of the valve:
The majority of the valve can be sustained, all superfluous parts are excluded, and in case of incomplete closure of the valve a synthetic ring is sewed to the valvular attachment. This procedure cannot be applied for completely destroyed valves or calcified valves.
Valvuar prosthesis
There are mechanical as well as biological valvular prosthesis. The mechanical ones are more durable, but require lifelong taking of certain medication (Marcoumar). Biological valves suffer from speedier calcification. For all bearers of valvuar prosthesis it is obligatory to take endocarditis prophylaxis in form of antibiotics in case of any injury or surgical procedure. All patients with such prosthesis will receive a document informing about the valvular prosthesis, which they are required to carry with them at all times.
Cardiac arrhythmia
An irregular heartbeat is the most frequent form of cardiac arrhythmia (atrial fibrillation). This condition is treated medicinally, where the most frequent medication for cardiac arrhythmia is Marcoumar. This type of cardiac arrhythmia is not life threatening, it can however have a limiting influence onto the physical performance. Occasionally, electrical conversion therapy (electroshock) is suggested.
For your information, normal pulse should range between 50 and 100 beats per minute and show certain regularity. A heart rate under 40 beats per minute (bardycardia) most frequently requires treatment with a pacemaker, while ventricular arrhythmia, when the heart rate exceeds average (ventricular tachycardia) requires a special type of pacemaker combined with a defibrillator (AICD).
Pacemakers
Pacemakers are implanted should the electrical system of the heart no longer be adequate. Reasons for this can be found on different ‘levels’ of the heart (sinus node, AV node, bundle of HIS etc). Procedures are usually performed under local anaesthesia. Thanks to modern techniques, pacemakers only weigh 20g and are implanted below the collarbone. The electrodes run ‘invisibly’ inside the veins into the heart. Depending on the disturbance, the heart needs impulses in the right ventricle (single chamber pacemaker) or in the atrium as well as the ventricle (dual-chamber pacemaker). Batteries are exchanged after 8 to 10 years. In case of severe cardiac insufficiency, a three chamber system might be needed, where a third electrode is implanted into the left ventricle.
AICD
An automated implantable cardio converter-defibrillator (AICD) limits fast life-threatening ventricular arrhythmia (originating from the ventricles) by an electrical impulse. At the same time heavy medication for stabilizing the heart rhythm will have to be taken on a continuous basis. Every patient with a pacemaker will receive a document informing about the existence of the pacemaker, which has to be carried at all times. Daily life is not influenced by the pacemaker; however heavy magnetic fields should be avoided (MRIs, security screening at the airport etc). Usage of mobile phones or cordless phones is possible.
High blood pressure (hypertension)
The World Health Organization (WHO) speaks of hypertension if systolic blood pressure is above 140mmHg or diastolic pressure is over 90 mmHg. High blood pressure is common in industrial countries – in the age group of fifty years and older every second person is affected by hypertension. The risk for high blood pressure increases with age, though even young people may already suffer from this disease, especially due to obesity and lack of exercise. This has led to a steady increase of children and youngsters with high blood pressure over the last years.
Initially, high blood pressure will not cause too many problems. Often the ones afflicted with hypertension are unaware of their condition; roughly 50% are ignorant to the fact that they are patients with high blood pressure. What makes it dangerous is the fact that even without symptoms damage to the heart, brain, kidneys and eyes continues. Uncontrolled high blood pressure increases the risk for heart attack, cardiac insufficiency, stroke, renal insufficiency, and loss of eye sight.
In the developed countries roughly half of all deaths are attributed to cardiovascular diseases. Frequently, hypertension is involved. This underlines the importance of preventive care. When diagnosed early and treated accordingly, onset of consecutive damage can be delayed if not avoided and life expectancy increases considerably.
Hypertension can be caused by disturbances of the hormone system, of the cardiovascular system as well as because of renal damage. In the majority of cases, the cause of high blood pressure is unknown. It can though be treated by different kinds of medication in combination with changes to your lifestyle to lower blood pressure and reduce the risk of complication.
Peripheral arterial occlusive disease (PAOD)
Peripheral arterial occlusive disease is a condition in which the blood supply of peripheral body parts, most commonly legs and occasionally the arms is restricted. This is caused by stenosis or blockage of the arteries which in turn is caused by arteriosclerosis. The restriction in blood flow results in less oxygen supply of arm and leg muscles. Physical activity (e.g. walking) increases the need for oxygen even more and pain may develop.
Since the underlying arteriosclerosis may not be limited to the extremities but affects all blood vessels of the human body, PAOD is commonly associated with coronary diseases, inadequate blood flow to the brain resulting in stroke. PAOD reduces life expectancy by about ten years.
Causes
Risk factors include cigarette smoking, diabetes, elevated blood lipid levels and high blood pressure.
Symptoms
POAD commonly causes pain the extremities in question. POAD of the legs is also referred to as intermittent claudication. People suffering from claudication have to stop every few meters due to muscle pain when walking.
Diagnosis
The complaints presented by the patient serve as first clue for diagnosing POAD. Diagnosis will be confirmed through oscillography, ultrasound exams, CT scans or MRIs.
Therapy options
Therapy options depend on the severity of the disease and range from medication to widening the vessels in question. If these fail, surgical interventions may be an option.
Stroke
A stroke causes serious damage to the brain, which happens if the blood supply to part of the brain is suddenly cut off. Causes
The most common cause of stroke occurs when a blood clot blocks the flow of blood, oxygen and nutrients to the brain. The brains cells in the part of the brain affected by the insufficient supply die soon after. The underlying cause is often arteriosclerosis, e.g. of the carotid artery but also of the smaller brain arteries. Another cause of stroke are blood clots that form in the left ventricle due to cardiac arrhythmia (atrial fibrillation). These clots travel up the blood stream towards the brain where they clog up vessels. Hemorrhages account for about 15 – 20% of all strokes. These hemorrhages occur when a blood vessel in the skull bursts, which can be caused by high blood pressure as well as congenital malformations of the arteries.
Among the symptoms of stroke are:
- sudden weakness or numbness of one leg or arm
- sudden drooping of the mouth (numbness of the face muscle)
- sudden slurred or garbled speech
- sudden change of consciousness, person appears confused
- sudden visual disturbances on one or both eyes (e.g. double images, blind spots)
- sudden dizziness, loss of balance or gait disorder
- extreme headache – especially in case of known high blood pressure
Treatment
If you suspect that you or someone else is having a stroke, immediately contact the emergency doctor or the ambulance. The faster blood flow of the brain can be re-established, the more brain tissue can be saved. Ideally first line treatment is done in a specialized stroke unit. Apart from the immediate treatment, early interdisciplinary measures such as physiotherapy or speech therapy are key.
Varicose veins
Varicose veins are enlarged irregularly running veins that usually occur on the legs but may also be seen in the pelvic area. Roughly 50% of all Europeans between the age of 25 to 74 are affected by varicose veins with its lumpy, bulging appearance. Even in its minimal form, known as spider veins, these harmless tiny enlarged veins are considered cosmetically undesirable.
Causes
Causes for varicose veins are manifold. Varicose veins of primary cause are generally caused by weakness in the wall of the vein. This may be hereditary and is often coupled with weakness of the connective tissue and the veins. Lack of exercise, obesity and prolonged standing at work are contributing factors. Women are more affected than men. The hormonal changes during pregnancy soften muscles and connective tissue but also the veins. Multiple pregnancies worsen the situation even more. As the uterus grows during gestation blood flow from the legs becomes more difficult.
Symptoms
Amongst the first symptoms we find heavy, tired, aching legs as well as swellings, which are noted after extended periods of standing or sitting. Discomfort is greater in menstruating women. The symptoms also worsen during warm weather and at the end of a long day. They may improve by rising up legs and cooling. Leg cramps are NOT typically considered to be related to varicose veins. Once the enlarged veins become visible under skin and bulge beneath the skin, the disease comes to the surface.
Diagnosis
You should consult your doctor when suspecting problems with the veins. Symptoms can be eased by simple methods, and early treatment avoids complications and worsening of the situation. A diagnosis is made based on the symptoms presented by the patients and their genetic disposition as well as physical exams and ultrasound tests.
Complications
Varicose veins can cause a number of complications. The enlarged vein may become inflamed. Frequently, blood clots form at the spot in question, which cause a blockage of the vein (varicophlebitis). This condition is quite painful, and the area affected will look red and feel hot. The clot may also travel into the deep veins, which increases the risk of lung embolism. If you experience unusual leg pain or swellings, it is advisable to seek immediate medical attention. In case of shortness of breath and chest pain contacting an emergency doctor or ambulance is required.
Severe varicose veins cause stress to the blood circulating in the superficial veins but in the long run also the deep veins will be affected by the large amount of blood. This may lead to chronic swellings (edema) of the leg. Skin problems and tissue damage, even ulcers may develop. The medical term for this ulcerated leg is ulcus cruris. The area around the ankle is mostly affected by these complications.
Varicose veins and ulcerated legs could also be caused by deep vein thrombosis, which describes a blockage of the deep vein blood flow due to a blood clot. Deep vein thrombosis usually occurs in the leg and pelvic area. Doctors refer to these as secondary varicose veins. Thrombosis of arm or should vein is less common.
Treatment
Patients often ask whether there is anything they can do to prevent varicose veins. The answer s is: under certain conditions, yes. A healthy lifestyle, controlling ones weight, endurance sports, vein gymnastics and cold showers of lower leg or knee area may be beneficial.
Mostly therapeutic measures will have already become necessary. An angiologist will assess the severity of your varicose veins and recommend treatment if needed. There are conservative as well as operative measures available, but the decision largely depends on the kind of disease, meaning the type of varicose veins and the extent. Treatment options include compression, scleroptherapy, laser treatment, radio wave therapy and surgical options.
Thrombosis
Thrombosis is the formation of a blood clot (thrombus) inside a blood vessel or the heart, which obstructs the blood flow. The fact that our blood has the ability to clot is very useful under normal circumstances, if we cut our finger for example. Our body immediately starts a sophisticated chain reaction to stop the bleeding. It provides blood cells and endogenous clotting agents to seal the wound and a scab is formed to allow healing.
Sometimes the blood may clot almost accidentally, without this being desired behaviour. A clot is formed at the wrong place at the wrong time. This clot partially or completely obstructs the blood flow.
Thrombosis may theoretically occur in any artery of the human body. Depending on which artery is affected, there are different consequences. If the clot has developed in an artery, we speak of arterial thrombosis which can cause heart attacks, strokes or cloggings of the leg arteries.
Venous thrombosis
There are two different kinds of venous thromboses: superficial venous thrombosis and deep vein thrombosis. Superficial venous thrombosis, also called vein inflammation, usually affects an enlarged bulging vein. The underlying cause for the thrombosis is the varicose vein disease. It may also affect a healthy vein – in this case this may be related to any other underlying severe disease.
Superficial venous thromboses are quite common and contrary to earlier believes, they are not entirely harmless. They may lead to deep vein thrombosis or pulmonary embolism. Patients who already had a superficial venous thrombosis tend to be at risk for another superficial venous thrombosis (relapse).
Superficial thromboses caused by varicose veins frequently come with complications. Therefore, early surgery is considered to be a preventive measure. During hot weather, a large number of patients with varicose veins suffer from severe superficial venous thrombosis.
Deep vein thrombosis is the formation of a blood clot within a deep leg vein. Immediate treatment is key and includes medication, compression socks or surgery, as well as dissolution of the thrombus (lysis) to avoid risk of pulmonary embolus.
Risk factors
There are numerous factors said to increase the risk of deep vein thrombosis, like extensive surgery, obesity, coagulation disorders, cancer, pregnancy, and contraceptive pills – especially in combination with smoking. Another substantial factor are varicose veins. Longer periods of inactivity, during bus tours for example, or on long haul flights may trigger deep vein thrombosis. Due to this, the disease has been termed ‘economy class syndrome’. The same holds true for extended periods of bed rest or immobilization of a limb with plaster. These factors increase the risk of suffering from deep vein thrombosis.
Symptoms
Thrombosis may present itself with varying complaints depending on which vessel is affected. Sometimes symptoms are completely absent or the signs only develop gradually over time. The following signs and symptoms point towards deep vein thrombosis: swelling of the leg in question, pain, the leg feels heavy and surprisingly warm. The skin on the affected leg may develop a bluish discoloration.
Diagnosis
Usually symptoms already point towards thrombosis. The doctor will have to confirm diagnosis through different investigative test by means of ultrasound for example.
Complications
If left untreated, thrombosis of leg or pelvic vein may result in a life-threatening condition called pulmonary embolism: parts of the blockage break off and travel via the blood stream into the lung vessels. Possible symptoms are shortness of breath, coughing, chest pain and heart palpitations. An extended pulmonary embolus is stress to heart and may result heart failure.
Therapy options
Frequently, anticoagulants are administered in thrombosis treatment. These are medicines which prevent clotting of the blood (coagulation inhibitors, blood thinners). In case of leg thrombosis customized compression socks will be prescribed. Lastly, there is the option of surgery or dissolution of the obstruction (lysis).